Adobe. (n.d.). Indian family having fun during Holi festival – Outdoor mother, son and daughter laughing in front of camera, summer-party and vacation concept (soft focus on mom face) [Stock photo]. Adobe Stock. Retrieved November 9, 2025, from https://stock.adobe.com/1536728443
Adobe. (n.d.). [Stock image 946607364] [Stock photo]. Adobe Stock. Retrieved November 9, 2025, from https://stock.adobe.com/946607364
bird_saranyoo. (n.d.). A Native American elder resting in a hospital bed, surrounded by caring family members offering love and support [Stock photo]. Adobe Stock. Retrieved November 9, 2025, from https://stock.adobe.com/1017338135
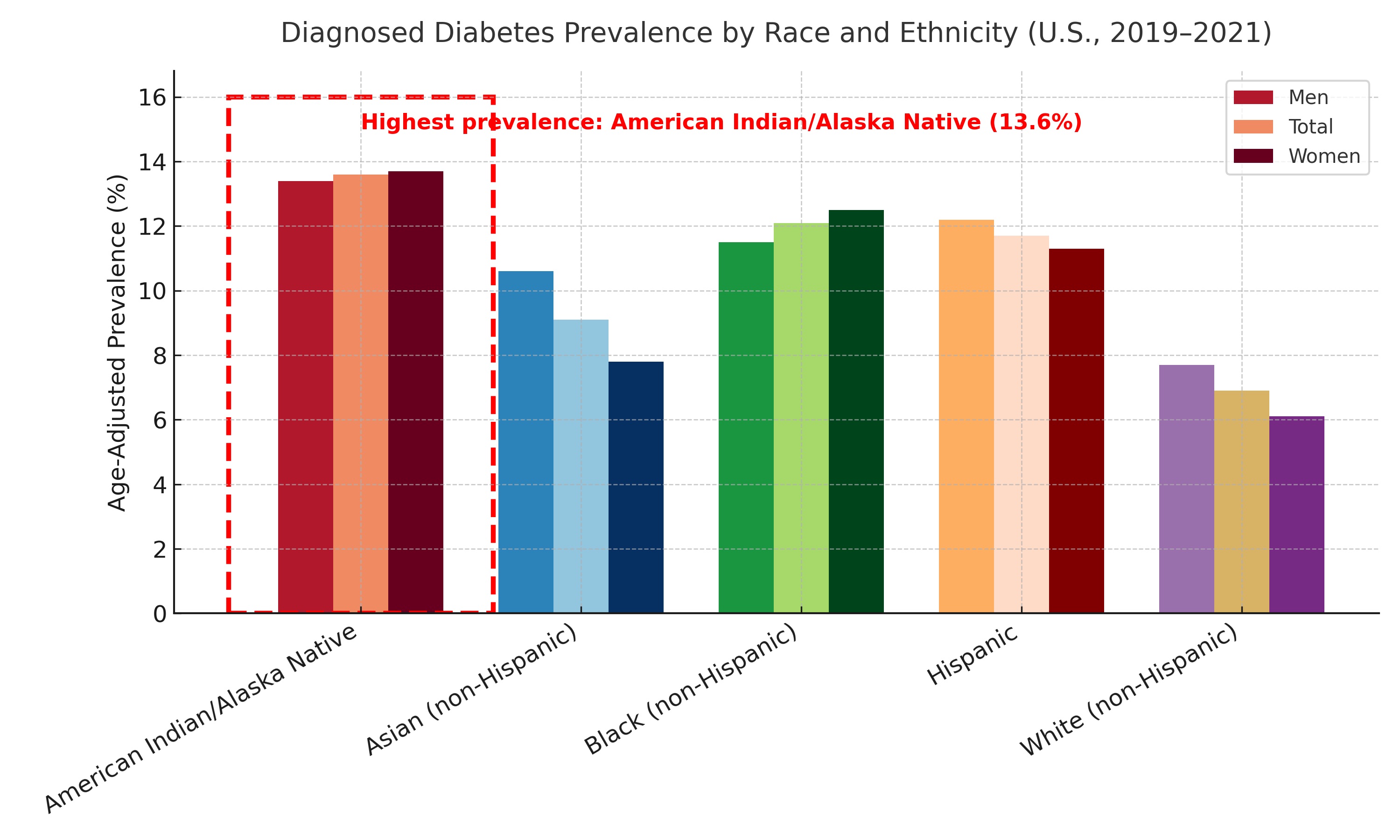
Centers for Disease Control and Prevention. (2024, May 15). Appendix A: Detailed tables. https://www.cdc.gov/diabetes/php/data-research/appendix.html#cdc_report_pub_study_section_3-table-3
David. (n.d.). A bundle of sage and an eagle feather are laid out in preparation of a Native American, Indian, or Indigenous smudging ceremony. Pemberton BC, Canada [Photograph]. Adobe Stock. https://stock.adobe.com/508544344
Erikson, E. H. (1982). The life cycle completed: A review. W. W. Norton & Company.
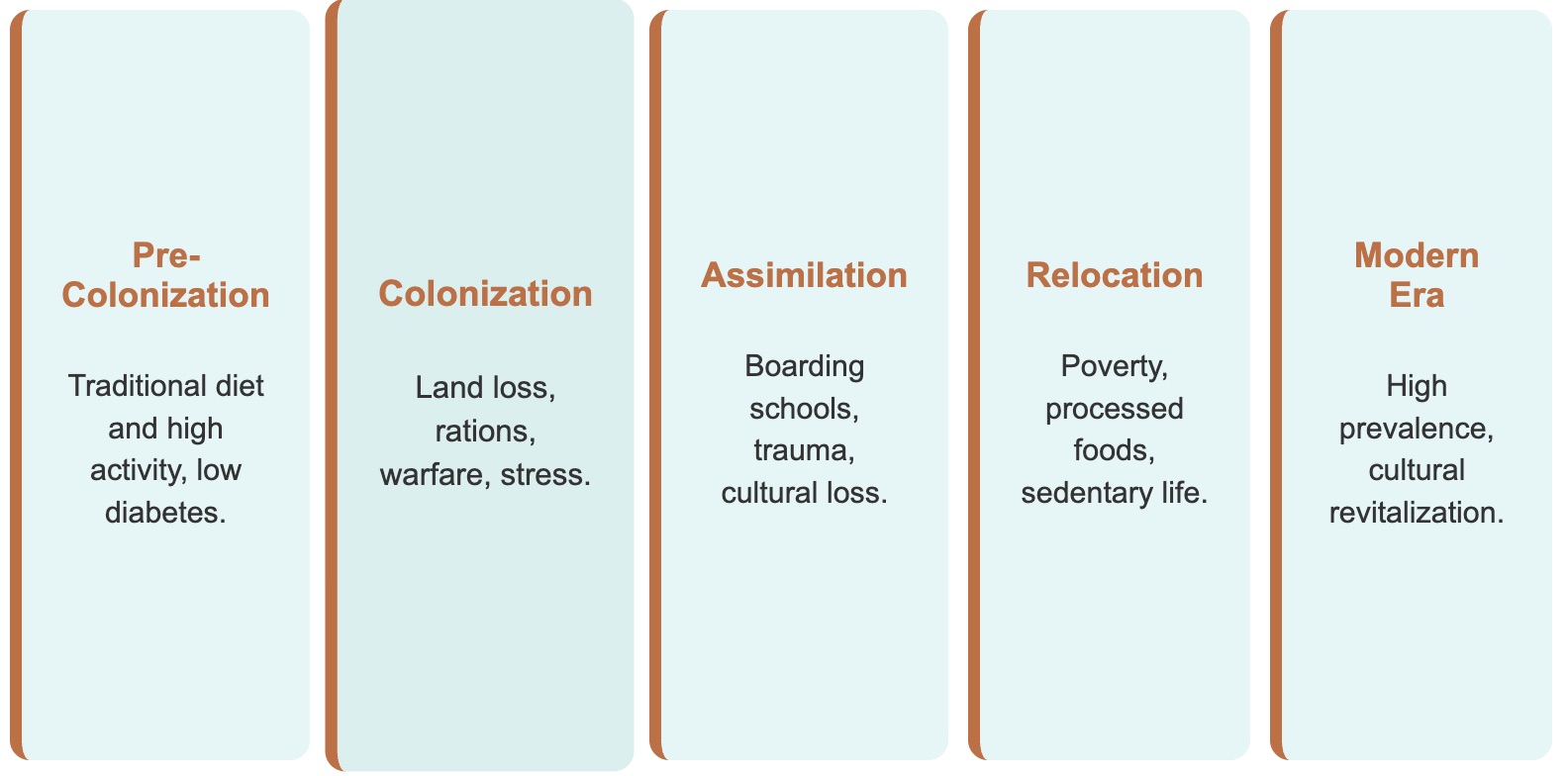
Gone, J. P., & Trimble, J. E. (2012). American Indian and Alaska Native mental health: Diverse perspectives on enduring disparities. Annual Review of Clinical Psychology, 8, 131–160. https://doi.org/10.1146/annurev-clinpsy-032511-143127
Indian Health Service. (2023). Disparities. U.S. Department of Health and Human Services. https://www.ihs.gov/newsroom/factsheets/disparities/
Indian Health Service. (2024). 2024 IHS diabetes care and outcomes audit results. U.S. Department of Health and Human Services. https://www.ihs.gov/diabetes/data/
Jernigan, V. B., D'Amico, E. J., Duran, B., & Buchwald, D. (2020). Multilevel and community-level interventions with Native Americans: Challenges and opportunities. Prevention Science, 21(Suppl 1), 65–73. https://doi.org/10.1007/s11121-018-0916-3
Moslow, M. (n.d.). Chic Medicine Wheel [Digital illustration]. Original artwork.
National Institute of Diabetes and Digestive and Kidney Diseases. (2023). Diabetes in American Indians and Alaska Natives. National Institutes of Health. https://www.niddk.nih.gov/health-information/community-health-outreach/american-indian-alaska-native
Office of Minority Health. (2023). Diabetes and American Indians/Alaska Natives. U.S. Department of Health and Human Services. https://minorityhealth.hhs.gov/diabetes-and-american-indiansalaska-natives
Special Diabetes Program for Indians. (2022). My Native Plate program materials. Indian Health Service. https://www.ihs.gov/diabetes/sdpi/
Stock 4 You. (n.d.). Portrait motivated executive confident senior business man specialist looking dreaming at copy space. Inspired Indian or Latin Hispanic mature middle-age boss, leader, CEO male businessman in office [Stock photo]. Adobe Stock. Retrieved November 9, 2025, from https://stock.adobe.com/1505937914
U.S. Department of Agriculture. (2021). Food access research atlas. Economic Research Service. https://www.ers.usda.gov/data-products/food-access-research-atlas/
Walls, M. L., & Whitbeck, L. B. (2012). The intergenerational effects of relocation policies on indigenous families. Journal of Family Issues, 33(9), 1272–1293. https://doi.org/10.1177/0192513X12447178
Wedekind, L. E., Mitchell, C. M., Andersen, C. C., Knowler, W. C., & Hanson, R. L. (2021). Epidemiology of type 2 diabetes in Indigenous communities in the United States. Current Diabetes Reports, 21(11), 47. https://doi.org/10.1007/s11892-021-01406-3